In 2017-2018, superstar Lady gaga opened up to the world about her struggle with rescheduling her concert tour dates due to widespread debilitating chronic pain and her Fibromyalgia diagnosis. She has continued to be courageous and raise awareness and connect with individuals living with this condition. Sometimes it is difficult to believe that this energetic artist performing all over the world suffers from this disorder. Let’s take some time to talk about this condition!
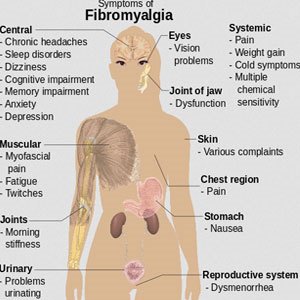
Fibromyalgia is a chronic health condition that can cause widespread musculoskeletal pain. Contrary to popular belief, it does not cause systemic inflammation and it is not considered to be an autoimmune disease. Individuals may have a chief complaint of symptoms such as tenderness to touch/pressure (for at least 3 months), severe fatigue, sleep disturbance or feeling unrefreshed from sleep, impaired memory or a reduced ability to think clearly (“foggy state” or “fibro fog”).
CONDITIONS THAT MAY BE SEEN WITH FIBROMYALGIA
In the clinical history, an individual may also report a personal history of conditions including:
· Migraine or tension headaches
· Anxiety and/or Depression
· Irritable bowel syndrome (IBS) or gastroesophageal reflux disease (GERD)
· Irritable or overactive bladder
· Pelvic pain
· Temporomandibular jaw pain
· Sleep disorders (Restless leg syndrome, sleep apnea)
DIAGNOSIS
Diagnosis is dependent on a subjective clinical history. There may be specific tender points on the body that are present on a physical exam.
A tender point exam is not required for a diagnosis.
There is no specific blood test or imaging to diagnose Fibromyalgia but often these are used to rule out other conditions with a similar presentation, like Hypothyroidism (under active thyroid), rheumatoid arthritis and lupus.
Remember, rheumatoid arthritis and lupus can cause inflammation in joints and various organs!!
RISK FACTORS
There is no known direct cause of Fibromyalgia, however certain factors are believed to increase the risk of development
· Gender: Women have a higher prevalence than men.
· Genetics: Certain genetic mutations may increase your risk of developing Fibromyalgia – but genes alone do not cause Fibromyalgia.
· Existing conditions: People with autoimmune disease including Lupus, Rheumatoid Arthritis are thought to be at an increased risk of developing Fibromyalgia. Osteoarthritis (“wear and tear arthritis”) may also be a factor.
· Stress/trauma: Physical trauma, like a car accident; emotional or psychological stress may also trigger Fibromyalgia.
A health care professional may monitor for depression and anxiety in individuals with Fibromyalgia because of the chronic pain and sleep problems that may be experienced with this condition.
TREATMENT
Although there is no cure for Fibromyalgia, medication, lifestyle modifications and alternative therapies may help relieve symptoms and improve quality of life.
· Physical Activity and exercise: low-moderate impact aerobic activity which strengthens muscles such as walking, cycling swimming, water aerobics, yoga and tai-chi can be beneficial in improving one’s quality of life.
Low impact exercise it is not harmful, although some pain may be experienced initially.
A patient should consult with a physician and or physical therapist to confirm what exercise regimen is best for the individual.
· Cognitive Behavioral Therapy may help an individual better comprehend how specific thoughts and behaviors may impact pain. CBT may result in stress and tenderness reduction.
· Diet and Nutrition: Lifestyle modifications can help improve symptoms by improving self-care.
Avoidance of excess alcohol
Limit caffeine and sugar , highly processed and fried foods
Ensure a diet rich with omega -3-fatty acidsEating fruits and vegetables that may contain antioxidants and natural chemicals in certain plant based food called phytochemicals that may aid in improving inflammation.
Adequate hydration
· Recognizing and identifying triggers for Fibromyalgia.
· Participating in activities that reduce stress and anxiety such as meditation, mindfulness, and deep breathing exercises are crucial.
· Correcting and enhancing sleep patterns can help reduce sleep disturbances and encourage relaxation.
REMEMBER:
1) Exercise regularly
2) Eat Healthy
3) Reduce stress
4) Drink water
5) Get More SleepThese lifestyle tips can benefit all of us in general!
ARE THERE MEDICAL TREATMENTS?
· Medications: There are some approved drugs to help treat Fibromyalgia and reduce pain by affecting specific chemicals in the brain.
Duloxetine (Cymbalta
Milnacipran (Savella)
Amitryptiline (Elavil).
Pregablin (Lyrica) or Gabapentin (Neurontin) impact the nerve cells that play a role in the pain transmission pathway.
Other medications such as acetaminophen (Tylenol), nonsteroidal anti-inflammatory drugs (NSAIDS) or cyclobenzaprine (Flexeril) may be useful to treat other causes of pain that can be seen with Fibromyalgia such as arthritis and muscle pain.
o Opiod narcotic medications and sleep medications such as benzodiaziapines should be avoided.
Your doctor will determine the best course of treatment depending on your individual presentation and clinical profile.
WHO TREATS FIBROMYALGIA?
A rheumatologist specializes in the treatment of musculoskeletal and autoimmune disease. As symptoms of Fibromyalgia often mimic some autoimmune diseases, it is often a rheumatologist who will evaluate the patient for other autoimmune diseases such as rheumatoid arthritis.
A primary care physician as well as other specialists such as a physiatrist, sleep medicine doctor, psychiatrist or therapist may be involved in creating a treatment plan aiming to help the patient self-manage their Fibromyalgia long term and continue monitoring an individual’s progress. This information is for educational purposes only, not as medical advice or as a diagnosis. Please see your physician should you have any questions, symptoms, or any concerns.
References:www.rheumatology.org,http://www.fmaware.org